Seen / Resources / Fertility Treatments / Embryo Grading Explained: What It Means for Your IVF Cycle
Embryo Grading Explained: What It Means for Your IVF Cycle
Embryo grading is a way embryologists assess the development and appearance of embryos during IVF to help decide which to transfer or freeze — but it’s not a verdict on your outcome. While a higher grade might suggest a stronger chance of success, many lower-grade embryos go on to become healthy babies.

Author

Reviewed by
Kayleigh Hartigan
28 min read
Updated 7 July 2025
Key takeaways:
- Embryo grading is a guide, not a guarantee. Grading helps clinics identify which embryos look most promising for transfer or freezing, but even lower-grade embryos can (and do!) lead to healthy pregnancies.
- Day 3 and Day 5 embryos are graded differently. Early-stage (Day 3) embryos are assessed by cell number and symmetry, while blastocysts (Day 5+) are evaluated based on expansion, inner cell mass, and outer cell layer quality.
- Higher grades often have better odds — but they’re not the only factor. Studies show that excellent- or good-quality embryos are more likely to implant, but success also depends on factors like genetics, uterine health, and how embryos behave after thawing. [1]
- Often, not every embryo is frozen. Clinics usually only freeze embryos that meet certain quality standards to maximise future success, but practices vary, so ask your clinic what they recommend for you.
What is embryo grading?
Embryo grading is a system embryologists use to assess the appearance and development of your embryos during IVF. It helps the clinic understand which embryos are most likely to implant successfully — and guides decisions around which to transfer, freeze, or continue monitoring.
Each embryo is looked at under a microscope, usually on Day 3 (when it’s around 6–10 cells) and again on Day 5 (as it develops into a blastocyst). Your embryologist will check things like how evenly the cells are dividing, whether there’s any fragmentation, and — at blastocyst stage — how well the inner and outer parts of the embryo are forming. It’s a detailed, skilled process, and no two embryos (or patients) are exactly alike. [2,3]
Grading helps your clinic decide which embryo(s) to transfer, how many to transfer (usually just one, as recommended by the HFEA), and whether to freeze any remaining embryos for future use.
It’s important to remember that embryo grading isn’t a prediction or a promise — and even embryos with lower grades can still become healthy babies.
How are embryos graded?
Grading takes place behind the scenes in the IVF lab, where a team of embryologists — scientists with specialist training in reproductive biology — observe your embryos with meticulous care. These are methodical, time-sensitive evaluations carried out under strictly controlled conditions, using high-resolution optics and inverted microscopes (a stereomicroscope) with high magnification designed to capture the tiniest shifts in structure, shape, and development. [4]
Alongside human expertise, some clinics are now using time-lapse imaging to take thousands of photos during an embryo’s development — giving embryologists a fuller picture of how each embryo grows, rather than a single snapshot in time. These images can then be analysed by artificial intelligence (AI) models, which are trained to spot patterns that may be invisible to the naked eye.
While AI isn’t a replacement for expert embryologists — and isn’t used in every clinic — it’s an evolving tool that could support more consistent grading and embryo selection in the future. Still, the final decisions are made by people who understand that an embryo is more than just a score. It’s a possibility — and sometimes, the ones that surprise us are the ones that go the distance.
Day 3 embryo grading
On Day 3, embryos are in the cleavage stage — meaning the single fertilised egg has divided into multiple individual cells, though the overall size hasn’t changed. Embryologists look at:
- How many cells the embryo has — ideally 6 to 10, with 8 often considered optimal
- Whether those cells are evenly sized — symmetry is seen as a good sign
- Fragmentation — small pieces of cell debris that may indicate less stable cell division
Grading is usually done on a scale of 1 to 4 or 5, with Grade 1 being the most symmetrical, least fragmented, and considered highest quality — but lower-grade embryos can still implant and develop into healthy pregnancies.
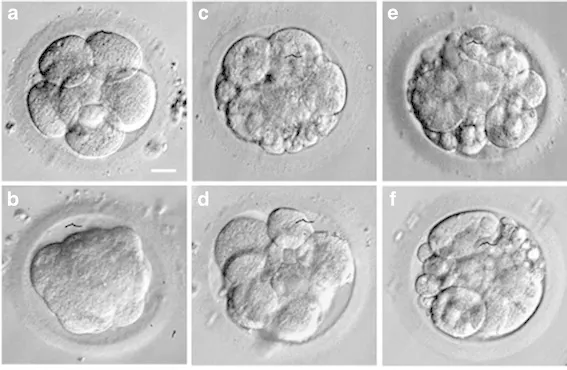
Image of a selection of day 3 embryos [5]
Day 5 embryo grading
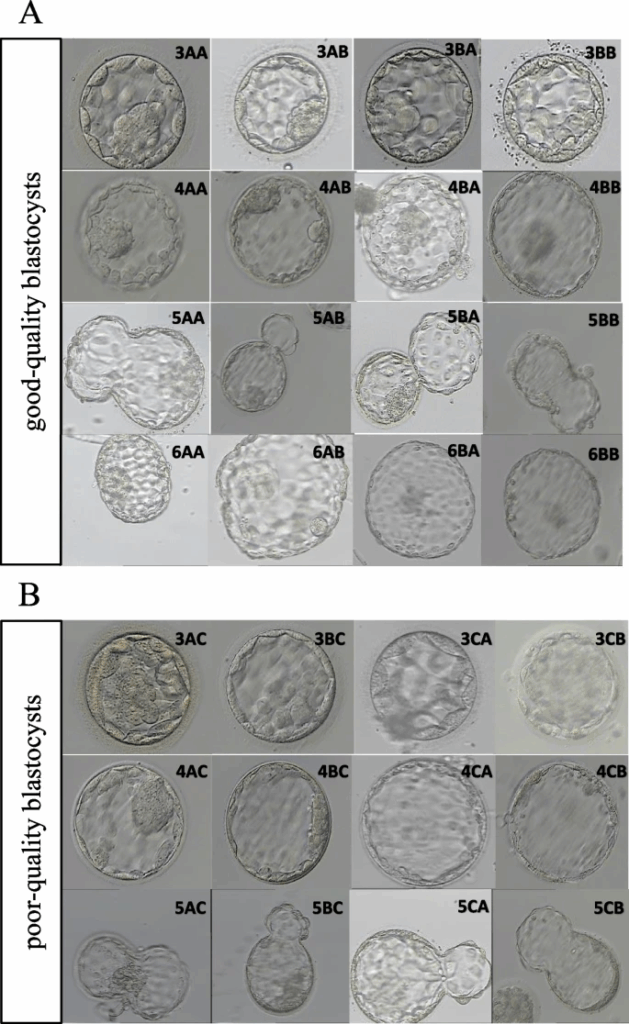
By Day 5, embryos that continue developing are known as blastocysts — and at this stage, there’s more detail for embryologists to assess. The embryo has now formed distinct parts, including the cells that could go on to become the baby and the placenta. To grade a blastocyst, embryologists focus on three main features:
- Blastocyst expansion (graded 1–6): This refers to how much the fluid-filled cavity inside the embryo (blastocoel) has expanded. A 1 means early development; a 6 indicates a fully hatched blastocyst that’s ready for implantation.
- Inner Cell Mass (ICM): This refers to the group of cells that will become the foetus, which is graded A to C:
- A — many tightly packed cells
- B — loosely grouped cells
- C — fewer, irregular cells
- Trophectoderm (TE): The outer layer that will form the placenta and supporting structures — this is also graded A to C:
- A — cohesive layer with many cells
- B — thinner or less uniform
- C — sparse or uneven cell distribution
Embryo grading and success rates
While it doesn’t assess genetic health, several studies suggest a meaningful association between an embryo’s grade and its potential to result in a clinical pregnancy or live birth — particularly when evaluating euploid embryos.
A euploid embryo is one that has the typical number of chromosomes — 46 in total — which is crucial for healthy development. Embryos with missing or extra chromosomes (known as aneuploid) are less likely to implant, and more likely to result in miscarriage. While grading can give a sense of how well an embryo is developing, it’s only when you combine it with genetic testing (typically PGT-A, more on that later) that you get a fuller picture of its potential. [7]
A 2018 retrospective study analysing 914 single euploid embryo transfers found that embryos classified as higher morphological quality were more likely to result in pregnancy and live birth: [8]
- “Excellent” quality embryos showed a 65% pregnancy rate and a 50% live birth rate.
- “Good” quality embryos showed a 59.3% pregnancy rate and a 49.7% live birth rate.
- “Average” quality embryos showed a 50.3% pregnancy rate and a 42.3% live birth rate.
- “Poor” quality embryos showed a 33.3% pregnancy rate and a 25% live birth rate.
When you receive your embryo report, you’ll usually see a combination of a number and two letters — something like 5AA, 4BB, or 3BC. This is your embryo grade, and it offers a snapshot of how that embryo looked under the microscope on the day it was assessed.
Below, you’ll find a comprehensive embryo grading chart showing every possible Day 5 blastocyst grade and their average success rate: [8]
49.7% live birth rate
42.3% live birth rate
25% live birth rate
42.3% live birth rate
25% live birth rate
25% live birth rate
25% live birth rate
25% live birth rate
25% live birth rate
49.7% live birth rate
42.3% live birth rate
25% live birth rate
42.3% live birth rate
25% live birth rate
25% live birth rate
25% live birth rate
25% live birth rate
25% live birth rate
50% live birth rate
49.7% live birth rate
42.3% live birth rate
49.7% live birth rate
42.3% live birth rate
25% live birth rate
42.3% live birth rate
25% live birth rate
25% live birth rate
50% live birth rate
49.7% live birth rate
42.3% live birth rate
49.7% live birth rate
42.3% live birth rate
25% live birth rate
42.3% live birth rate
25% live birth rate
25% live birth rate
50% live birth rate
49.7% live birth rate
42.3% live birth rate
49.7% live birth rate
42.3% live birth rate
25% live birth rate
42.3% live birth rate
25% live birth rate
25% live birth rate
50% live birth rate
49.7% live birth rate
42.3% live birth rate
49.7% live birth rate
42.3% live birth rate
25% live birth rate
42.3% live birth rate
25% live birth rate
25% live birth rate
What is PGT-A?
Preimplantation Genetic Testing for Aneuploidy (PGT-A) is an optional add-on during IVF where a few cells are carefully biopsied from a blastocyst and tested in a lab to check for chromosomal abnormalities. This helps identify which embryos are euploid — and may be more likely to lead to a healthy pregnancy. [7]
PGT-A doesn’t guarantee success, and it isn’t right for everyone. But for some patients — especially those who’ve experienced recurrent miscarriage or have had multiple unsuccessful IVF cycles — it can help prioritise which embryo to transfer first.
Do frozen embryos have different grading considerations?
Yes — while frozen embryos are initially graded in the same way as fresh embryos, their post-thaw appearance and behaviour can influence how they’re reassessed and prioritised for transfer.
A large 2024 study of over 7,700 single euploid embryo transfers found that changes in embryo morphology after thawing were significantly associated with live birth outcomes. Embryos that maintained their original grade after thaw had the highest live birth rate (55.8%). [9]
In contrast:
- Embryos that were downgraded after thawing showed a lower live birth rate (47.5%)
- Those that did not re-expand — meaning they failed to reabsorb fluid and resume development — had the lowest live birth rate (26.6%)
- Embryos that appeared to improve in grade after thawing had even higher odds of success than those that stayed the same
This suggests that embryo behaviour after thawing — particularly re-expansion and morphological changes — may be just as important as the original grading at the time of freezing. While pre-freeze grades are still useful for planning, embryologists often re-evaluate embryos on the day of transfer to determine their current viability.
So, although grading systems are consistent, frozen embryos are given an additional layer of assessment — not just based on what they looked like going into storage, but how they respond after thawing. This dynamic response is a key consideration in clinical decision-making and can impact the timing and outcome of your embryo transfer.
If you’re preparing for a frozen embryo transfer, your clinic may reassess your embryo on the day to help guide whether it’s the best candidate for transfer at that time.
Can you tell gender by embryo grading?
No — embryo grading cannot accurately predict the sex of an embryo. While there may be developmental trends linked to sex, grading is not a reliable indicator of gender and should not be used to infer it. [10]
The link between gender and embryo grading
Some small studies have noted a correlation between faster-developing embryos and male sex chromosomes. For instance, in one study of over 500 blastocysts screened using comprehensive chromosome testing, a higher proportion of the most morphologically advanced embryos (grades 5AA and 6AA) were male. Meanwhile, embryos that progressed more slowly (grade 3 or below) were more likely to be female. But it’s worth noting that this was based on a small sample size, and needs more research before we can definitively say whether it’s true or not. [11]
This reflects a difference in developmental timing, not in embryo quality or viability. Male embryos may, on average, reach blastocyst stage slightly faster than female embryos — but this is not a universal rule, and it does not apply consistently across cycles or patients.
If embryo sex is medically or personally relevant, the only accurate method of determining it is through preimplantation genetic testing for aneuploidy (PGT-A). PGT-A allows embryologists to identify embryos with the correct number of chromosomes, and in doing so, it can reveal sex chromosomes (XX or XY). This process is optional, and only available through IVF where embryo biopsy is performed.
Embryo fragmentation and how it factors into embryo grading
Fragmentation is one of the key elements embryologists assess when grading embryos in IVF — but what it actually means, and how much it matters, isn’t always straightforward.
In simple terms, fragmentation refers to small pieces of cell cytoplasm that break off from developing cells (blastomeres) in the early embryo. These fragments don’t contain nuclei (so they’re not whole cells) and are usually considered a sign that something in the embryo’s development isn’t going entirely to plan. [12]
You might see this mentioned in a lab report or embryo quality summary as “cytoplasmic fragmentation” — and it’s typically used as a marker of how likely an embryo is to develop well and implant successfully. That said, not all fragmentation is created equal.
Why does fragmentation matter?
Fragmentation is typically used as a marker of embryo quality, because it can reduce the amount of healthy cytoplasm and essential organelles available to support cell division. The more fragmentation there is, especially if it’s widespread or uneven, the more likely it is that the embryo’s development might slow down — or stop altogether. [12]
That’s why embryos with high levels of fragmentation often receive lower grades in IVF. These grades help embryologists decide which embryos are most likely to develop into blastocysts, implant successfully, and lead to a pregnancy.
Is fragmentation always bad?
Not necessarily. A low level of fragmentation (generally under 10–15%) is fairly common and often doesn’t affect how an embryo develops. Even moderate fragmentation can be tolerated, especially if the embryo is dividing at a healthy pace and the cells are uniform in size. [12]
In fact, recent research using time-lapse imaging has shown that fragments can be dynamic — they might move, reabsorb, or change during development. Some embryos with early fragmentation go on to self-correct, forming healthy blastocysts and resulting in successful pregnancies. [12]
What really matters is context:
- How much fragmentation is present
- When it occurs
- How it’s distributed (scattered vs concentrated)
- What the rest of the embryo looks like — including symmetry, cell number, and division rate
So while severe fragmentation (often >35–50%) is usually a sign that implantation could be less likely to happen, mild or well-contained fragmentation isn’t an automatic dealbreaker.
What causes fragmentation?
Fragmentation is likely caused by a mix of factors, including:
- Sperm or egg quality [13]
- Chromosomal abnormalities [13]
- Suboptimal lab conditions like oxidative stress or low oxygen [13]
- Disruptions in how the embryo’s cells divide and organise themselves [14,15]
But there’s still a lot we don’t know. Fragmentation may be the embryo’s way of managing stress or damage — which means it could be a sign of resilience, not just weakness.
The difference between embryo grading and embryo genetic testing (PGT-A)
Embryo grading and preimplantation genetic testing for aneuploidy (PGT-A) are often talked about as if they’re two sides of the same coin — but they actually look at totally different aspects of an embryo’s potential. Understanding how they work together (and sometimes contradict each other) can help you and your fertility clinic team make clearer decisions about which embryo to transfer, especially if you’ve got multiple to choose from.
- Embryo grading is a visual assessment — it’s based on how the embryo looks under a microscope. Specifically, the embryologist scores the quality of the inner cell mass (which will become the fetus) and the trophectoderm (which will become the placenta). It gives a sense of how well the embryo has developed so far.
- PGT-A, on the other hand, goes beneath the surface. It looks at the genetic makeup of the embryo — whether it has the correct number of chromosomes. Unlike embryo grading — which is a visual assessment of how an embryo looks — PGT-A offers an insight that can’t be seen under a microscope. [7]
Can a genetically normal embryo still be poor quality?
Yes — and it happens more than you’d think. A euploid (chromosomally normal) embryo might still be graded as “fair” or “poor” based on its structure. Equally, an embryo that looks beautiful under the microscope might come back from PGT-A with a chromosomal issue. That’s because morphology doesn’t always reflect genetics. [16]
What should you prioritise if you have both grading and PGT-A?
If an embryo has been tested and confirmed euploid, genetics takes priority. But grading still matters. Studies consistently show that among euploid embryos, those with higher morphology grades — especially in the trophectoderm — are more likely to implant and result in a live birth. [17,18]
If an embryo isn’t tested, grading gives you your best clue about which one to transfer first.
If an embryo is confirmed to be euploid, grading can help guide which one to prioritise — and your clinic team will support you in making that decision based on your unique situation.
AI and other embryo selection tools
Embryo grading is one of the most important — and most subjective — steps in IVF. Traditionally, embryologists assess embryos by looking at them under a microscope and assigning a grade based on how they appear, like cell number, symmetry, and development stage. It’s a skill that requires experience and training, but it’s still inherently limited by human perception.
This is where AI and other technologies like time-lapse imaging are starting to reshape the process. Rather than relying solely on a single visual snapshot, time-lapse systems capture thousands of images as the embryo develops, offering a fuller picture of how it grows and changes over time. AI models can then analyse these images alongside clinical data to predict which embryos are most likely to result in a pregnancy — not just based on static appearance, but on patterns that might be invisible to the human eye.
In systematic reviews, AI has shown higher accuracy than embryologists when predicting embryo quality and implantation outcomes, especially when combining visual data with clinical factors like age or hormone levels. This suggests a shift from traditional embryo grading toward more data-driven embryo selection — not to replace embryologists, but to support them in making more consistent, personalised decisions. [19,20,21]
Still, it’s early days. While these tools show promise, they’re not yet widely regulated or standardised, and not all clinics offer them. If you’re comparing fertility clinics, it’s worth asking whether technologies like AI or time-lapse imaging are part of their grading process.
Questions to ask your fertility clinic about embryo grading
When your clinic shares your embryo grades, it can be a lot to take in — especially if it’s your first IVF cycle. The terminology can feel technical, the stakes feel high, and you may not know what’s helpful to ask. But knowing the right questions can turn a confusing report into a clearer picture of what’s going on, and what your options might be.
Here are some thoughtful questions to consider when speaking to your embryologist or consultant:
Can you explain how my embryos were graded and what those grades mean?
Ask for this in plain language. What do the letters or numbers refer to? What’s considered a strong embryo — and what might be more uncertain?How does this grading system relate to the chance of a live birth?
Grading doesn’t guarantee an outcome, but it’s one part of assessing potential. Ask how your specific grades link to what they see in clinical outcomes.Were my embryos assessed using AI or time-lapse imaging?
Some clinics use advanced technologies alongside human assessment. Understanding what tools were used — and whether they impact how decisions are made — can be helpful context.Are there any embryos you would recommend transferring or freezing over others? Why?
This gives insight into how the team is prioritising based on quality, development stage, or potential genetic testing results.Do you expect these embryo grades to influence my treatment plan going forward?
For example, would the grades change how many embryos might be transferred, or whether further testing or another cycle is recommended?How do these embryo grades compare to others you typically see in people my age or with my fertility profile?
Sometimes it’s reassuring — or grounding — to hear how your results fit into the wider picture.
You’re well within your rights to take notes or ask for a summary in writing. If something doesn’t make sense, keep asking — your clinic is there to support you. Most embryologists are genuinely passionate about what they do — and usually more than happy to talk you through the details. Don’t hesitate to take notes or ask for things to be explained again. Understanding your embryo grading isn’t just your right — it’s something your clinic wants for you too.
Accessibility to embryo grading
Access to detailed embryo grading isn’t guaranteed for everyone — and that can feel frustrating when you’re trying to make informed decisions about your fertility path.
Some clinics routinely share detailed reports, photos, and videos of embryo development. Others may only provide basic grading, or explain it verbally. This often depends on the clinic’s approach, the technology they use, and whether you’re being treated privately or via the NHS. In many NHS-funded cycles, for example, grading information may be limited and access to add-ons like time-lapse imaging or preimplantation genetic testing (PGT) isn’t always included.
Cost can also be a barrier. Advanced tools that help assess embryo quality — such as PGT-A or AI-supported grading — often come with a price tag. And while these technologies can offer more data, they’re not always necessary or available to everyone. But they aren’t essential, and not having access to them won’t necessarily impact your outcome. If they’re not right for you, financially or otherwise, that’s not a problem.
If you want more help figuring out which fertility clinic could be the best fit for you, our community reviews can offer valuable insight into how different providers handle embryo grading, communication, and patient care — from people who’ve been there.
Embryo grading FAQs
Does a better grade mean a better chance of success?
Higher embryo grades generally reflect stronger visual and developmental qualities, which can increase the likelihood of implantation — but they are not a guarantee. Success depends on many factors, including the age of the egg, the uterine environment, and overall health. While grading offers valuable guidance, it is not the sole predictor of outcome.
Is 4AA or 5AA embryo better?
A 4AA and 5AA embryo are both considered excellent quality, with the numbers referring to the stage of expansion (4 = expanded blastocyst, 5 = hatching blastocyst) and the letters grading the inner cell mass and trophectoderm. Neither is inherently “better” — both have strong implantation potential, and your clinic will recommend the most suitable option based on your individual situation, not just the grade.
Are grade A embryos more likely to implant?
Grade A embryos typically reflect excellent appearance in the lab, but it’s important to understand that implantation depends on much more than visual grading alone. While statistically they may show stronger potential, not every Grade A embryo leads to pregnancy — and many lower-grade embryos still result in healthy births.
Does embryo grading affect baby health?
While embryo grading is primarily designed to predict the chance of implantation and pregnancy success, recent research has also explored whether embryo quality influences long-term health outcomes for the baby. Some studies suggest that embryos graded as “poor quality” may carry slightly higher risks of congenital anomalies, musculoskeletal differences (such as talipes), or chromosomal anomalies compared to “good quality” embryos. Other research has linked poor-quality embryos in frozen cycles with higher odds of low birth weight or preterm birth. [22,23]
However, it’s essential to view these findings in context. While there are statistical associations, most babies born following assisted reproduction — regardless of embryo grade — are healthy. Many factors, including underlying parental health, treatment specifics, and natural biological variation, can influence outcomes. Fertility clinics evaluate the whole clinical picture, not just the lab grading, when advising on embryo transfer decisions.
Can poor quality embryos become healthy babies?
Yes — poor quality embryos can become healthy babies.
Although they may have a lower chance of implanting compared to good-quality embryos, studies show that once a poor-quality embryo implants and establishes a clinical pregnancy, its chances of leading to a live birth are similar to those of higher-graded embryos. Embryo appearance (morphology) doesn’t always reflect genetic health — meaning even embryos that look less promising in the lab can still carry the potential to grow into healthy children. While the odds may be lower overall, a poor-quality embryo is not without hope. [24,25]
What grade embryos can be frozen?
Not every embryo gets frozen — and which ones do depends on both their quality and your clinic’s protocols.
Generally, fertility clinics aim to freeze only embryos that are graded “excellent”, good”, or “average” based on their development stage (whether they’re early-stage, cleavage-stage, or blastocysts). This is because these embryos are more likely to survive freezing and thawing and lead to a successful pregnancy later. Clinics want to maximise your future chances, so they typically avoid freezing embryos that look too poor in quality, as their survival and success rates tend to be lower.
That said, grading systems can vary, and the decision is individualised. If you have questions about whether your specific embryos can be frozen — and why — it’s always worth having an open conversation with your clinic team.
What if my embryo isn’t top grade?
Embryo grading can feel daunting, particularly when your embryo isn’t considered “top grade.” But it’s important to understand what that grading really represents — and what it doesn’t.
A lower grade doesn’t mean your embryo is “bad” or incapable of leading to a healthy pregnancy. Grading is a visual assessment of how the embryo appears at a certain point in time, and while it offers useful insights, it doesn’t account for everything. Many factors influence the potential for implantation and live birth, including embryo genetics, uterine environment, and individual response to treatment. In fact, many lower-grade embryos have resulted in successful pregnancies.
If you’ve been given a grading you didn’t expect, you’re not alone. It’s completely valid to want more clarity. Your fertility clinic will help you understand what your embryo’s grade means in the context of your treatment plan.
Sources
- https://www.sciencedirect.com/science/article/pii/S2666571922000032
- https://www.hfea.gov.uk/treatments/explore-all-treatments/decisions-to-make-about-your-embryos/
- https://www.cuh.nhs.uk/patient-information/laboratory-guide-for-patients/
- https://www.frontiersin.org/journals/veterinary-science/articles/10.3389/fvets.2024.1364570/full
- https://www.researchgate.net/publication/306416397_Different_effectiveness_of_closed_embryo_culture_system_with_time-lapse_imaging_EmbryoScopeTM_in_comparison_to_standard_manual_embryology_in_good_and_poor_prognosis_patients_A_prospectively_randomized
- https://link.springer.com/article/10.1186/s12884-023-05387-x
- https://www.hfea.gov.uk/treatments/treatment-add-ons/pre-implantation-genetic-testing-for-aneuploidy-pgt-a/
- https://www.fertstert.org/article/S0015-0282(16)63012-1/fulltext
- https://pubmed.ncbi.nlm.nih.gov/38580183/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8490581/
- https://www.sciencedirect.com/science/article/pii/S001502821000600X
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11092204/
- https://www.sciencedirect.com/science/article/pii/S0015028207010333
- https://academic.oup.com/humrep/article-abstract/15/12/2621/2915860
- https://academic.oup.com/humrep/article-abstract/17/9/2415/563980
- https://academic.oup.com/humrep/article/39/Supplement_1/deae108.871/7703473
- https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2022.858042/full
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6345636/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10426717/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8324599/
- https://www.frontiersin.org/journals/artificial-intelligence/articles/10.3389/frai.2024.1375474/full
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7243353/
- https://www.sciencedirect.com/science/article/abs/pii/S1472648319306686
- https://link.springer.com/article/10.1186/s40738-020-00072-5
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10573848/


