Seen / Resources / Fertility Treatments / Donor Egg IVF: What to Expect at Every Stage
Donor Egg IVF: What to Expect at Every Stage
Donor egg IVF is a well-established fertility treatment that helps people who can’t use their own eggs to build their families — whether due to age, medical reasons, or genetics. This guide explains how it works, who it’s for, what to expect, and what to consider before starting treatment.

Author
Tassia O’Callaghan

Reviewed by
Kayleigh Hartigan
22 min read
Treatment spotlight:
- Donor egg IVF is a form of assisted reproduction that uses eggs from a screened donor, fertilised with sperm, to help someone become pregnant.
- It’s often recommended when using your own eggs isn’t possible or carries a high genetic risk — including for older patients, those with early menopause, or LGBTQ+ families.
- A single cycle typically takes 6–9 weeks, though matching with a donor or using frozen eggs can change the timeline.
- Most UK clinics now offer frozen donor egg IVF, which has slightly lower birth rates than fresh cycles but greater availability and simpler logistics. [1]
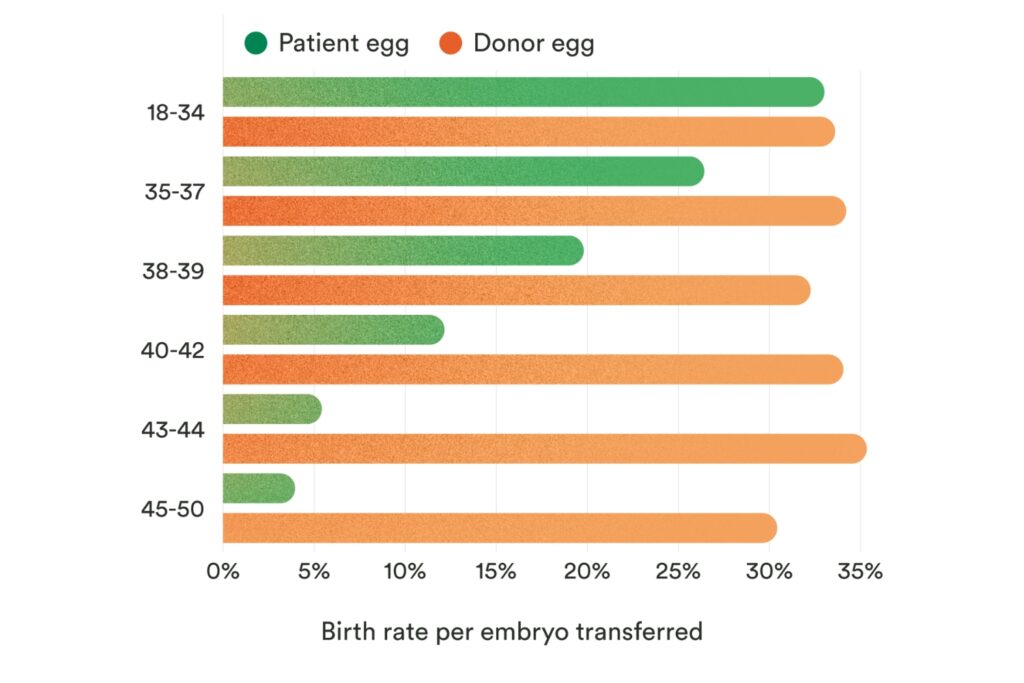
- Success rates are consistently higher than IVF with a patient’s own eggs, averaging over 30% per embryo transfer across all age groups. [2]
- Costs are usually higher than standard IVF, averaging around £10,374 per private cycle, and NHS access depends on local eligibility rules. [3]
- Emotional and legal factors — like future donor disclosure — are an important part of planning and are often supported with counselling.
What is donor egg IVF?
Donor egg IVF is a fertility treatment where eggs from a donor are used to help someone become pregnant. It’s an option when using your own eggs isn’t possible or recommended.
In this process, eggs from a carefully screened donor are fertilised with sperm (from a partner or donor), and the resulting embryos are transferred into the uterus of the intended parent or a surrogate. These donor eggs may come directly from a fertility clinic or be sourced from a dedicated egg bank, either in the UK or internationally. The donor has no legal or parental rights to any child born, and all donors in the UK are thoroughly screened for health and genetic conditions. [4]
Treatment Essentials: IVF
Learn more about IVF: explore the steps involved, how much it costs, understand success rates and risks – all in one convenient, in-depth guide.
Who is donor egg IVF for?
Donor egg IVF is a treatment option for individuals and couples who are unable to conceive using their own eggs. This may include those experiencing age-related infertility, early menopause, poor ovarian reserve, or repeated IVF failure. It is also recommended in cases where there is a significant risk of passing on a genetic condition from the person who would normally provide the egg.
Importantly, donor egg IVF is not limited to heterosexual couples. It is also used by single parents and LGBTQ+ families — including same-sex male couples working with a surrogate — who require donor eggs to build their families. [2]
How popular is donor egg IVF?
Donor egg IVF has become an increasingly important and widely used fertility treatment. In the UK, national data shows that donor conception (which includes egg, sperm, and embryo donation) now accounts for around one in every six IVF births — reflecting a steady rise in demand over recent decades.
According to the Human Fertilisation & Embryology Authority (HFEA), over 4,100 children were born in 2019 using donor sperm, eggs, or embryos. Since 1991, more than 70,000 donor-conceived children have been born in the UK. [2]
There are also more donor eggs available than ever before in the UK, with new egg donor registrations increasing from approximately 500 in the early 90s to around 1,500 in the late 2010s. [5]
Before you start treatment, remember:
- The legal considerations: In the UK, donor-conceived children have the legal right to access identifying information about their donor once they turn 18. Thinking ahead about how — and when — you’ll talk to your child about their origins is an important part of planning. [4]
- The emotional impact: Using donor eggs can bring up a wide range of feelings — from grief over genetic connection to questions around identity, bonding, and family storytelling. Many people find that these emotions evolve over time, and that counselling can help them feel more grounded and ready for treatment.
- Check clinic experience and success rates: Not all clinics are the same. According to the HFEA, success rates using donor eggs in people aged 43–50 rise from just 5% (with their own eggs) to over 30% — but outcomes can still vary by clinic and approach. Look for a clinic with experience in donor treatments, robust donor matching processes, and transparent data on success rates. [2]
- Discuss with your partner or support network: This is rarely a solo decision, even if you are pursuing treatment on your own. Partners, family, friends, or counsellors can help you navigate the emotional landscape and provide the support you’ll need before, during, and after treatment. There are also fertility charities that either specialise in donor egg IVF, or have a group for donor egg IVF support, such as Fertility Network UK, Donor Conception Network, Donor Conceived UK, and the British Infertility Counselling Association.
- Consider financial planning: Donor egg IVF is usually more expensive than standard IVF — not just because of the treatment itself, but because you’re also covering the cost of donor eggs. In the UK, a private donor egg IVF cycle averages £10,374, but this can vary widely depending on the clinic, the type of donor (fresh or frozen), and what’s included. NHS-funded donor treatments are available but limited, with only 13% of donor cycles funded compared to around 40% of standard IVF cycles (HFEA, 2016–2020 data). Understanding your budget, funding options, and any additional costs (such as donor matching or embryo storage) will help you plan more confidently. [5]
IVF with donor egg process: step by step
While every donor egg IVF journey is unique, most follow a structured process (similar to traditional IVF) designed to give you the best possible chance of success. The steps vary slightly depending on whether you’re using fresh or frozen donor eggs — and it’s important to know the difference. Fresh cycles require coordinating your treatment with the donor’s, so not all clinics offer them due to the logistics involved. Most UK clinics now use frozen donor eggs, which are retrieved in advance and stored for future use.
Here’s what to expect at each stage:
Step 1: Pretreatment
Time: 2–6 weeks
Location: Clinic
First, you’ll meet with your fertility specialist for consultations, blood tests, and scans. These help assess your overall health and prepare a treatment plan tailored to your needs.
At the same time, the clinic will guide you through the process of selecting and matching with an egg donor.
- With frozen eggs, you’ll select from a pre-retrieved and cryopreserved batch, often making the process quicker and more flexible.
- With fresh eggs, the donor will begin ovarian stimulation specifically for you — this adds extra time and coordination, and may not be offered by all clinics.
Many clinics work directly with external egg banks or source donor eggs through partnerships. Some have their own in-house banks, while others may coordinate with national or international egg banks, giving you access to a wider range of donors (though sometimes at a higher cost). It’s also possible to approach an egg bank independently and then match with a clinic to carry out the treatment.
While you’re not undergoing stimulation yourself, you’ll start hormone treatment to prepare your uterus, ensuring it’s ready for embryo transfer later. This typically involves oestrogen and progesterone, either as tablets, patches, or injections.
Step 2: Egg retrieval from donor
Time: ~2 weeks
Location: Clinic
During this phase, the donor undergoes ovarian stimulation. They will take medications to encourage multiple eggs to mature, followed by a minor surgical procedure to retrieve them.
This step only applies if you’re doing a fresh donor egg cycle. If you’re using frozen eggs, they’ve already been collected and are thawed when ready for fertilisation — often through an egg bank working with your clinic.
Step 3: Fertilisation and embryo culture
Time: 3–5 days
Location: Clinic
Once retrieved (fresh) or thawed (frozen), the donor eggs are fertilised with either yours, your partner’s sperm, or donor sperm in the laboratory. The resulting embryos are carefully monitored as they grow, typically reaching the blastocyst stage (day 5–6) before transfer.
If you have surplus high-quality embryos, they can usually be frozen for future use — a valuable option if you’re planning to try again or grow your family later.
Step 4: Embryo transfer
Time: 1 day
Location: Clinic
An embryologist will select the most promising embryo to transfer into the uterus of the person who will be carrying the pregnancy. This is a quick, generally painless procedure that typically doesn’t require anaesthesia. A thin catheter is passed through the cervix, and the embryo is gently placed inside.
Step 5: Wait for pregnancy test
Time: ~2 weeks
Location: Home
About two weeks after transfer, you’ll return to the clinic or take a blood test at home to check for pregnancy.
Clinics often recommend emotional support or counselling during this phase, as it can be one of the most emotionally intense parts of the process. Whatever the outcome, know that you are not alone — and there are always next steps and options ahead.
How long does donor egg IVF take?
Typical timeline: 6-9 weeks or longer per donor egg IVF cycle, depending on how long it takes to find a suitable egg donor
If you’re using frozen donor eggs, the timeline may be slightly shorter, as the donor matching and stimulation steps have already been completed. However, it’s important to remember that unexpected factors — such as donor availability or additional screening — can sometimes add extra time.
Understanding donor egg IVF success rates
Donor egg IVF offers consistently higher success rates compared to IVF using a patient’s own eggs, particularly for those in their late 30s, 40s, and beyond. According to the Human Fertilisation & Embryology Authority (HFEA), the live birth rate per embryo transfer using a patient’s own eggs drops sharply with age — averaging just 5% for people aged 43–50. But when donor eggs are used, success rates stay steady at over 30% across all age groups. [2]
Why the difference? It’s largely because egg donors are typically younger (with an average age of 31) and screened for fertility health, meaning the eggs themselves are more viable, regardless of the age of the person carrying the pregnancy. This gives people whose own egg quality has declined — or who cannot use their own eggs for medical or genetic reasons — a significantly higher chance of achieving a pregnancy. And considering the average age of IVF patients was 36 years old, that’s often considered to be around the age that egg quality and quantity can potentially decline. [5,6]
While these numbers show that donor egg IVF can be effective, it’s important to remember that success rates can still vary between clinics. Reviewing a clinic’s data, understanding their approach, and discussing your individual circumstances with a specialist will give you the clearest picture of your personal chances. [5]
Why does donor egg IVF fail sometimes?
Even though donor egg IVF offers higher success rates compared to IVF using a patient’s own eggs — especially for those over 40 — it’s important to understand that no fertility treatment can guarantee pregnancy. Several factors, beyond the quality of the donor eggs, can affect the outcome. [2]
Here’s why donor egg IVF can sometimes fail:
- Embryo quality and genetics: While donor eggs typically come from young, healthy donors, not every egg will fertilise or develop into a high-quality embryo. Embryos may have chromosomal abnormalities that prevent implantation or lead to miscarriage. This is true even with younger eggs, although the risk is significantly lower compared to older eggs. That’s why many fertility clinics recommend genetic testing (PGT-A) on the eggs beforehand. [7,8]
- Uterine factors: A successful pregnancy requires not just a healthy embryo but also a receptive uterine lining. Conditions like fibroids, polyps, adhesions, or chronic endometritis can reduce the chances of implantation. Even if the uterus appears normal on scans, its “receptivity” — the window during which it can accept an embryo — may vary. However, there are tests that can check the uterine lining, such as the Endometrial Receptivity Test (also known as ERA testing). [9,10]
- The genetic match of the foetus: Some recent studies have suggested that for cases where the foetus is more closely related to the person carrying the pregnancy (for example, using a family member’s egg), “the maternal body may be more tolerant of a developing embryo that is genetically related to her”. However, it’s difficult to verify this theory, since often times, with donor egg IVF, there are often other factors at play, such as maternal age and low fertility. [11]
- Lifestyle and health factors: Although the eggs come from the donor, the health of the person carrying the pregnancy still plays a role. Factors like high BMI, smoking, excessive alcohol use, or poorly managed medical conditions (e.g., diabetes, thyroid disorders) can all reduce the chances of success. Making healthy lifestyle adjustments can support better outcomes. [12]
- Unexplained factors: Sometimes, even when everything looks optimal on paper, the cycle does not result in pregnancy. This is why clinics often recommend counselling alongside treatment, to help patients process uncertainty and cope with disappointment.
How common is miscarriage with donor eggs?
Unfortunately, miscarriage with donor eggs is fairly common. As the success rate (meaning live births) with donor egg IVF is around 30-35%, that means that the remaining 65-70% unfortunately either don’t implant (which means technically no pregnancy took place) or a miscarriage, which includes chemical pregnancies.
What if donor egg IVF doesn’t work?
If your donor egg IVF cycle doesn’t result in pregnancy, you still have options — and you are not alone. What you choose next depends on factors like your age, health, treatment history, and budget.
Here are some paths to consider:
- Frozen embryo transfer (FET): If you have embryos in storage, a frozen transfer may be your next step. On average, people undergo three embryo transfers before a live birth. [13]
- Further investigations: Your clinic might recommend reviewing uterine health, considering immunological or genetic testing, adjusting sperm source, or using a different donor.
- Exploring other options: You might decide to look into surrogacy, adoption, or other family-building routes.
- Taking a break or stopping: Stepping back can help you recover physically and emotionally. If you choose to stop treatment, support systems and counselling can help you navigate that decision.
Fresh vs. frozen donor egg IVF
If you’re considering donor egg IVF, one key decision is whether to use fresh or frozen eggs — and both options come with strong success rates.
According to the Human Fertilisation and Embryology Authority (HFEA), the birth rate per treatment cycle using frozen donor eggs is around 30%, only slightly below the 33% birth rate for fresh donor eggs (based on UK data from 2016). [1]
Why are both so effective? Much of it comes down to the fact that donor eggs — whether fresh or frozen — are typically from younger, carefully screened donors, giving them a fertility advantage over using a patient’s own eggs, especially for recipients in their 40s. For example, among people aged 43–45, frozen donor eggs offer significantly higher success rates than treatment with their own eggs.
Fresh cycles may offer a slightly higher birth rate, but most UK clinics now use frozen donor eggs due to simpler logistics and faster treatment timelines. Frozen eggs are typically sourced from egg banks — which are separate from clinics — and offer access to a wider pool of donors, including international options. While some clinics still offer fresh cycles, these require synchronising your cycle with the donor’s and are less commonly available. The right choice depends on your clinic’s offering, the egg bank they work with, and your personal priorities.
What are the risks of donor egg IVF?
While donor egg IVF is considered a safe and well-established treatment, it’s important to understand the potential risks so you can make informed choices. Here’s what to keep in mind:
- Multiple pregnancy risk: Transferring more than one embryo increases the chance of twins or more — and with it, a higher risk of complications like premature birth, gestational diabetes, or late miscarriage. UK clinics typically recommend single embryo transfer to lower these risks. [14,15]
- Pregnancy complications: As with all IVF pregnancies, there’s a slightly higher chance of pregnancy-related conditions like hypertension (high blood pressure) and gestational diabetes. Research also shows that donor egg pregnancies carry a higher risk of preeclampsia — a serious condition that needs medical attention. [16,17,18,19]
- Miscarriage risk: While miscarriage can still happen, using donor eggs (which typically come from younger donors) is associated with lower miscarriage rates compared to using your own eggs at an older age.
- Procedural risks (for the donor): Although you, as the recipient, won’t undergo egg retrieval, it’s worth knowing that donors face small but real risks like Ovarian Hyperstimulation Syndrome (OHSS) and surgical complications. [20]
- Financial and legal risks: While clinical care in the UK is highly regulated, going abroad or using imported donor eggs can carry additional uncertainties, including fewer guarantees around donor limits or long-term traceability. It’s essential to work with licensed, transparent providers to minimise these risks. [5]
- Emotional and psychological impact: Some people experience feelings of grief or disconnection because the baby won’t share their genetic material. Counselling and open discussion with your partner or support network can help navigate these feelings.
Is donor egg IVF available on the NHS?
Yes — but it’s not guaranteed everywhere. NHS funding for donor egg IVF depends on where you live (your local Integrated Care Board, or ICB) and whether you meet the local eligibility criteria. [21,22,23,4]
Here’s what you need to know:
- Age matters: In many areas, you may qualify if you’re under 40 and have been trying to conceive for at least two years, or have gone through 12 cycles of artificial insemination (including at least six intrauterine insemination or IUI cycles). Some areas may fund one cycle for people aged 40–42.
- Your health and lifestyle may count: Some ICBs set conditions, such as being a healthy weight or a non-smoker, and they may not fund treatment if you or your partner already have children.
- How long you’ve been trying to conceive: This length of time depends on your local ICB, an can range from a year to two years without a pregnancy. For some ICBs, even unsuccessful pregnancies can restart the clock again.
- Donor egg IVF is typically accessed through IVF funding: If your NHS funding is approved, the use of donor eggs is often included, especially in cases like premature ovarian failure, after cancer treatment, or when there’s a high risk of passing on an inherited condition. But availability can vary, and waiting lists can be long — particularly if you need a donor of a specific background.
- Initial tests may be covered: Even if you’re not eligible for funded IVF, you may entitled to NHS investigations to explore the cause of infertility.
If you’re considering NHS donor egg IVF, your GP is the best first contact. They can explain your local policies, refer you for testing, and guide you through next steps.
How much does donor egg IVF cost?
The cost of donor egg IVF in the UK can vary widely, but most private clinics charge between £9,000 and £15,000 per cycle, with an average cycle cost of £10,374. This base price usually covers the IVF treatment itself, but there are several important additional costs to be aware of. You’ll typically need to pay extra for donor matching (if you’re using an anonymous donor sourced through a clinic or egg bank), fertility medications (both for the donor to stimulate egg production and for the recipient to prepare the uterine lining), and frozen embryo storage if you’re planning to keep any remaining embryos for future use.
How Much Does IVF Cost in the UK?
Private costs for IVF in the UK vary greatly, ranging from £3,735 to £13,408 for an advertised IVF package. We break all of this down for you and more in our handy guide.
Source: Seen Fertility’s Treatment Essentials: IVF guide
Where can I find a donor egg IVF clinic?
The best place to start your search is with Seen Fertility’s Find a Clinic tool, where you can explore clinics across the UK. This isn’t just a directory — each clinic is scored based on real experiences from our community, with transparent details on costs, outcomes, and patient reviews to help you compare confidently.
For a more personalised approach, try our Clinic Match Tool, which allows you to filter clinics by your specific medical, emotional, and financial needs. You can shortlist your favourites, track them in your account, and even contact clinics directly — all at no extra cost.
It’s important to understand that IVF clinics and egg banks are not the same. You’ll first need to find a clinic that offers donor egg IVF — many work exclusively with frozen eggs, and only some offer fresh cycles due to the complexity of synchronising treatment with a donor. Once you’ve chosen a clinic, you’ll then need to access donor eggs. This can happen in a few ways:
- Some clinics source eggs through an external egg bank, and you’ll be billed through the clinic — often with a markup.
- Some clinics run their own in-house egg banks, which can limit choice but simplify logistics.
- Others will ask you to select and purchase donor eggs directly from a partner or independent egg bank (including international ones).
The setup varies from clinic to clinic and can affect both the availability of donor profiles and the overall cost of treatment. Seen Fertility will soon be launching a dedicated egg bank directory to help you compare options more easily.
If you’re already part of the Seen Fertility community, you can log in anytime to revisit your saved clinics. As you search, we recommend looking for HFEA-licensed clinics with well-established donor programs and clear information about how they source eggs.
Summary
Donor egg IVF offers options for people who can’t use their own eggs, whether due to maternal age, genetics, or family structure. With carefully screened donors and higher success rates, especially for those over 40, it’s a well-established treatment — but one that comes with emotional, financial, and medical considerations.
From choosing the right clinic and egg bank to understanding costs and risks, being informed helps you move forward with confidence. And with tools like Seen Fertility, you don’t have to navigate it alone — you can compare, plan, and find the right support for your unique path.
Donor egg IVF FAQs
Will my baby look like me if I use donor eggs?
Genetically, your baby inherits traits from the egg donor and the sperm source, not from you. But here’s what the research and lived experience show: feeling like your child’s parent isn’t determined by genetics alone.
Studies of mothers who used donor eggs reveal that most feel deeply bonded to their babies — often from pregnancy or birth — and that this sense of connection grows stronger over time. Some parents describe a “claiming” process, where pregnancy, birth, and day-to-day caregiving build the emotional foundation that makes a child yours. [24]
Is a donor egg pregnancy high risk?
No, a donor egg pregnancy isn’t automatically considered “high risk,” but there are a few extra factors worth being aware of.
Because donor egg recipients are often older (many are over 40) or have gone through complex fertility treatments, doctors may recommend closer monitoring. Age-related risks like high blood pressure, gestational diabetes, or placenta complications can be slightly more common — but these are not guaranteed and depend heavily on your individual health.
If you’re carrying one baby, are generally healthy, and have no major medical conditions or pregnancy complications, you may still be classified as “low risk.” This means your pregnancy and birth could be just as straightforward as anyone else’s. But if you have factors like a previous caesarean, twins, high BMI, or pre-existing health issues, your care team may recommend extra precautions. [25]
How do I prepare my body for IVF donor egg?
Preparing for donor egg IVF involves creating a healthy environment for pregnancy, both physically and emotionally.
Typically, people take daily folic acid (400 micrograms) to reduce the risk of neural tube defects and vitamin D (10 micrograms) to support bone and nervous system development. Vitamin A supplements are usually avoided because excessive amounts can be harmful. [26,27]
Lifestyle habits often play a role in outcomes. Smoking and alcohol use have been linked to lower success rates, and caffeine intake is commonly limited to under 200 mg per day (about two small cups of coffee). A balanced diet — high in vegetables, fruits, whole grains, lean proteins, and healthy fats — has been associated with positive effects on fertility treatment outcomes. [26,27]
Regular physical activity can help maintain strength and manage stress, while a body mass index (BMI) between 19–30 is generally considered optimal for treatment and pregnancy health. Existing medical conditions like diabetes, epilepsy, or hypertension are usually stabilised before treatment begins, often in coordination with healthcare teams. [26,27]
The emotional side is also significant. Many people experience complex feelings around donor egg IVF, including questions about identity, connection, or the future. Counselling and emotional support are common parts of preparation, helping individuals process these emotions as they move toward treatment. [27]
Your clinic will also advise on your protocol (drug programme), regularly monitoring your response to the treatment, so they can best advise you on how else you can prepare your body (and mind) for donor egg IVF. It’s important that you’re honest with your fertility doctors, so they can give you the most accurate information and advice they can. [28]
Sources
- https://www.hfea.gov.uk/about-us/news-and-press-releases/2018/press-release-age-is-the-key-factor-for-egg-freezing-success-says-new-hfea-report-as-overall-treatment-numbers-remain-low/
- https://www.hfea.gov.uk/about-us/news-and-press-releases/2022/rise-of-egg-and-sperm-donation-ends-heartache-for-thousands-says-uk-regulator/
- https://wordpress-998807-3515629.cloudwaysapps.com/fertility/treatment/ivf/
- https://www.hfea.gov.uk/treatments/explore-all-treatments/using-donated-eggs-sperm-or-embryos-in-treatment/
- https://www.hfea.gov.uk/about-us/publications/research-and-data/trends-in-egg-sperm-and-embryo-donation-2020/
- https://www.hfea.gov.uk/about-us/publications/research-and-data/fertility-treatment-2021-preliminary-trends-and-figures/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5330984/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7005195/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3510376/
- https://www.hfea.gov.uk/treatments/treatment-add-ons/endometrial-receptivity-testing/
- https://www.sciencedirect.com/science/article/abs/pii/S0378378224001415
- https://www.nhs.uk/conditions/infertility/
- https://www.hfea.gov.uk/about-us/publications/research-and-data/fertility-treatment-2018-trends-and-figures/
- https://www.hfea.gov.uk/about-us/our-campaign-to-reduce-multiple-births/
- https://www.hfea.gov.uk/about-us/publications/research-and-data/multiple-births-in-fertility-treatment-2019/
- https://www.sciencedirect.com/science/article/abs/pii/S0378378224001415
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5951714/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10165528/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6434532/
- https://www.hfea.gov.uk/treatments/explore-all-treatments/risks-of-fertility-treatment/
- https://www.nhs.uk/conditions/infertility/treatment/
- https://www.uhcw.nhs.uk/ivf/egg-donation/
- https://www.nhs.uk/tests-and-treatments/ivf/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7192012/
- https://www.bsuh.nhs.uk/maternity/wp-content/uploads/sites/7/2016/09/Next-baby-info.pdf
- https://www.newcastle-hospitals.nhs.uk/services/fertility-treatment/ivf-and-icsi-information-for-patients-having-treatment/preparation-for-pregnancy/
- https://www.bupa.co.uk/newsroom/ourviews/guide-prepare-body-ivf
- https://www.newcastle-hospitals.nhs.uk/services/fertility-treatment/egg-recipient-treatment/