Seen / Resources / Fertility Treatments / Antral Follicle Count (AFC) Testing Explained: How Clinics Measure Ovarian Reserve
AFC Testing Explained: How Clinics Measure Ovarian Reserve
Wondering what your antral follicle count means for your fertility? This guide breaks down everything you need to know about AFC: how it’s measured, what’s considered normal, and why it matters when planning or preserving your fertility.

Author
Tassia O’Callaghan

Reviewed by
Kayleigh Hartigan
18 min read
Updated 31 July 2025
Spotlight:
- AFC is a key fertility test that helps assess your ovarian reserve — the number of eggs you might have available at a given time. It’s often part of a Fertility MOT alongside AMH and FSH blood tests. [1]
- Antral follicles are small, fluid-filled sacs in your ovaries that contain immature eggs. These follicles (2–10mm in size) are visible on a transvaginal ultrasound and counted to calculate your AFC. [2]
- The scan can be done at any point in your cycle, though many clinics prefer days 2–5. It’s quick, usually takes 10–15 minutes, and provides an immediate snapshot of your egg supply. [3]
- Your AFC result may influence treatment plans, especially for IVF. A higher count may mean more eggs retrieved or a condition like PCOS (Polycystic Ovary Syndrome), while a lower count may guide medication choices or flag possible conditions like POI (Premature Ovarian Insufficiency). [4]
- A ‘normal’ AFC changes with age — for example, the average 35-year-old might have 8–15 follicles across both ovaries. Your individual count may differ, but it still offers useful clinical insights. [5]
- AFC works best when seen in context, alongside age, AMH, hormone health, and your overall fertility picture. It doesn’t predict when you’ll conceive, but it can help guide the right next steps. [6]
What is AFC in fertility?
AFC stands for antral follicle count. It’s one of the key ways fertility specialists assess ovarian reserve — that’s the number of eggs you’re working with at a given point in time. An antral follicle count (AFC) ultrasound is usually part of a broader fertility assessment — often referred to as a Fertility MOT — alongside blood tests like AMH (and sometimes FSH). Together, these checks help build a more detailed view of your ovarian reserve and any potential factors that could impact your fertility. [7]
AFC doesn’t predict your natural fertility or your ability to get pregnant without support — many people with a low count do conceive without intervention. But when it comes to assisted conception, it can help shape decisions around medication doses or eligibility for certain types of treatment (like NHS-funded IVF, where some clinics use a threshold of 4 follicles or more). [8]
AFC is often considered alongside other hormone markers like AMH and FSH, but age remains the most significant factor. That’s because egg quantity and quality both decline over time, particularly after 35 — something AFC can help illustrate, but not change. That said, understanding your AFC can bring clarity and confidence to your fertility path, whether you’re trying now or thinking about the future. [6]
What are antral follicles?
Antral follicles are small, fluid-filled sacs in your ovaries that contain immature eggs. They’re part of the natural cycle of egg development — and by the time a follicle reaches the antral stage, it’s visible on an internal ultrasound. Not every antral follicle will make it to ovulation, but they’re an important signpost of ovarian reserve and hormone activity. The number of antral follicles you have at a given time (your AFC) can help fertility specialists understand more about your egg supply and how your ovaries may respond to treatment. [2]
How is antral follicle count tested?
Antral follicle count (AFC) is measured using a transvaginal ultrasound — a type of scan that offers a close-up look at your ovaries. This is usually done before ovulation, when the small resting follicles (called antral follicles) are most visible, but can be done at any time in your cycle. Each follicle appears as a tiny black bubble on the screen, and the clinician will count how many they can see in each ovary. [3]
The scan itself takes place in a clinic and involves inserting a small ultrasound probe into the vagina. While this might sound a little daunting, it’s a routine and quick procedure — usually lasting around 10–15 minutes — and most people describe it as slightly uncomfortable rather than painful. You don’t need to fast or do anything special beforehand, though you may be asked to avoid intercourse or certain medications before the appointment depending on your clinic’s protocol. [8]
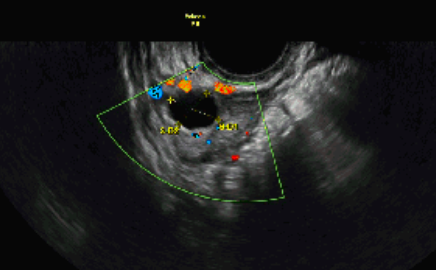
Image of an antral follicle count ultrasound — an ovary showing 3 follicles (highlighted in red and yellow).
Source: Tassia O’Callaghan
Treatment Essentials: Testing AMH Levels
Why do I need to do an antral follicle count scan?
An antral follicle count scan helps your fertility team understand how your ovaries are working right now. By checking how many small follicles are visible early in your cycle, they can get a clearer picture of your egg reserve and how your body might respond to certain treatments.
This scan is especially important if you’re being considered for ovulation induction, IVF, or NHS-funded treatment, where specific criteria often apply. It can guide medication choices, reduce the risk of complications like overstimulation, and help avoid delays by ensuring you’re on the right protocol from the start.
Can I ask my GP for an AFC test?
You can ask your GP about an antral follicle count (AFC) test, but whether it’s available to you on the NHS depends on your local ICB (Integrated Care Board) and their specific referral criteria. Some areas offer AFC scans as part of initial fertility investigations, while others only approve them once you’ve been referred to a specialist. If you’re over 35 or have been trying to conceive for a while, it’s worth bringing this up during your appointment — especially if you’re hoping to access NHS-funded fertility treatment down the line.
If you’re not eligible through the NHS or would prefer to take matters into your own hands, you can book an AFC scan privately. Many fertility clinics offer standalone assessments, including ultrasound and hormone testing, without needing a GP referral. You can use our Clinic Match tool to find a clinic that suits your needs, location, and budget.
When should an antral follicle count ultrasound be done?
An antral follicle count ultrasound can usually be done at any stage of your menstrual cycle — including during your period — because the small resting follicles it measures are present throughout. That said, many clinics prefer to schedule the scan in the early part of your cycle, typically between days 2 and 5, when hormone levels are more stable and the ovaries are easier to assess. If you’re not having regular periods, your clinic may suggest timing based on other factors or medications. [9]
Antral follicle count test before fertility treatment
Before starting fertility treatment, your clinic will likely recommend an antral follicle count test to help plan your care more effectively. It’s often one of the first steps before IVF, giving insight into how your ovaries are likely to respond to stimulation medication. This can shape everything from your drug dose to the number of monitoring appointments you’ll need during your cycle. [3]
There’s also a link between antral follicle count and IVF success. While it’s not the only factor, people with a higher count often produce more eggs during treatment, which can increase the number of embryos available for transfer or freezing. But quality matters too — and age, underlying health, and sperm factors also play a role. So while your antral follicle count for IVF offers important clues, it’s just one part of a bigger picture your team will look at when tailoring your treatment plan. [4,10,11,12,13]
Antral follicle count and underlying conditions
Antral follicle count (AFC) isn’t just useful for planning fertility treatment — it can also give insight into underlying health conditions that affect the ovaries, now or in the future. For example, people with endometriosis — particularly ovarian endometriomas, a type of cyst that develops when endometriosis affects the ovaries — often show a lower AFC on scans. This doesn’t always mean they’ll produce fewer eggs in IVF, but it can make interpretation more complex, especially if the follicles are hard to visualise. Knowing your AFC in this context can help clinicians set realistic expectations and tailor treatment with greater care. [14,15]
On the other end of the spectrum, people with polycystic ovary syndrome (PCOS) typically have a high AFC. This is one of the diagnostic criteria for PCOS, though thresholds can vary depending on the ultrasound equipment used. A high AFC doesn’t necessarily mean better fertility — it’s about context. In PCOS, it can reflect hormone imbalance and irregular ovulation, which may require specific management. [16,17]
A low AFC can also be a flag for conditions linked to earlier menopause or primary ovarian insufficiency (POI). Research shows that people with an AFC of 4 or fewer may be nearly twice as likely to experience menopause sooner than average — even when accounting for age, hormone levels, or smoking. Genetics can play a role here too, especially in cases of POI, where variants in genes involved in follicle development and ovarian function may impact AFC long before menopause symptoms appear. [18,19]
In short, your AFC can do more than inform fertility planning — it can help spotlight broader reproductive health patterns that deserve attention and support.
What is a ‘normal’ antral follicle count?
Defining what counts as a “normal” antral follicle count isn’t always straightforward — because every body is different. But looking at population data can offer helpful context. The table below gives an idea of what’s considered a normal antral follicle count by age, based on research involving women with proven fertility. Keep in mind: your result might fall outside these ranges and still be clinically appropriate for your individual situation. [5]
Age
Average follicle count
Low follicle count
High follicle count
25
16-34
<12
>25
30
13-22
<10
>22
35
8-15
<8
>18
38
7-13
<6
>15
40
4-7
<4
>12
45
1-4
<2
>8
What is the normal AFC in each ovary?
A normal antral follicle count per ovary typically ranges from 4 to 10 follicles, though this can vary depending on your age and overall ovarian reserve. In research involving women with proven fertility, the average count was about 4 follicles per ovary in the early follicular phase. This means a combined total of around 8 antral follicles across both ovaries is considered normal for many — but what’s normal for you may look slightly different. [5]
Find the right clinic for you
Choosing a clinic is one of the biggest decisions you’ll make. We’ll find the best options for you and arrange your pre-treatment tests, empowering you from this point onwards.
What does a ‘low’ antral follicle count mean?
A low antral follicle count (AFC) means fewer small, fluid-filled follicles were seen on your ultrasound — depending on your age. While this doesn’t mean you can’t get pregnant, it does suggest a reduced ovarian reserve, which may affect how your body responds to fertility treatment like IVF, and how many reproductive years you may have left. [20]
Clinically, a low AFC is linked to retrieving fewer eggs during stimulation, and there’s a higher chance of needing higher doses of medication or facing cycle cancellation. That’s because AFC is one of the most reliable tools we have for estimating ovarian response — it can be more predictive than hormone tests like AMH or FSH alone. [9]
It’s important to understand that AFC reflects quantity, not quality. People with a low count can still produce healthy, fertilisable eggs. Your age, overall health, and treatment approach also play a big role in your chances of success.
How to increase antral follicle count
Right now, there’s no strong or clinically proven way to increase your antral follicle count. Some early studies are exploring potential approaches — but most of the research is limited, small-scale, or inconclusive. While these findings may seem hopeful, there’s currently no significantly credible evidence that AFC can be increased through any specific treatment, lifestyle change, or supplement.
That said, here’s a look at what’s being explored — not as recommendations, but as areas of ongoing interest:
Selenium and vitamin E
In one small triple-blind study involving just 70 participants, people with signs of premature ovarian insufficiency took a daily supplement of selenium (200mcg) and vitamin E (400 IU) for 3 months. A year later, those who took the supplements had a significantly higher AFC compared to the placebo group. The supplements were well-tolerated, but because of the small size of the study, we don’t yet know if these results apply more broadly. [21]
Increasing dairy protein
A separate study of 265 women found no overall link between total protein intake and AFC — but it did find that higher dairy protein intake (around 2.3 cups of milk a day or more) was associated with a lower AFC. This was most noticeable in people who had never smoked. While this doesn’t prove that dairy causes a lower count, it may be worth exploring your diet with a fertility-aware nutritionist if you’re trying to optimise ovarian health. [22]
LH supplementation in specific cases
In a case report of two women with hypothalamic amenorrhoea (HA), daily or alternate-day doses of recombinant LH over one to two months led to increased AMH levels, improved AFC, and more mature eggs retrieved during IVF. This type of intervention is highly individualised and only relevant for certain diagnoses — but it highlights how hormonal support may benefit ovarian development in very specific scenarios. [23]
DHEA supplementation
DHEA (dehydroepiandrosterone) is a hormone that’s sometimes used in fertility treatment, particularly for people with diminished ovarian reserve. A few small studies suggest it might increase AFC or egg yield during IVF, especially in women over 35 or those with low AMH. But evidence is mixed, and it’s not suitable for everyone — so always speak to your clinic before trying it. [24,25,26]
Acupuncture
A recent exploratory randomised controlled trial found that acupuncture — when done before IVF — may improve oocyte yield in people with poor ovarian response (POR), particularly those over age 37 or undergoing multiple rounds of IVF. Those who received 16 sessions of targeted acupuncture showed a significantly higher number of mature eggs retrieved compared to those who did IVF alone. While the study was small and exploratory, it suggests that acupuncture could support ovarian function by improving blood flow, regulating hormones, and potentially reducing the decline seen with repeated IVF cycles. There’s currently no strong evidence that acupuncture can increase antral follicle count (AFC), but it may help reduce stress by lowering cortisol and supporting overall hormonal balance. As always, it’s worth discussing with your clinic to see if it might be right for your situation. [27,28,29]
Body weight
While AFC itself may not change dramatically with body size, research suggests that hormonal markers of ovarian reserve — like AMH and inhibin B — can be lower in people with a higher BMI. This doesn’t necessarily mean reduced egg count, but it can affect how your test results are interpreted. Reaching and maintaining a weight that supports hormone balance (without extremes) may help give a clearer picture of your ovarian health. If you’re unsure what’s right for you, your clinic can offer tailored guidance. [30]
At this stage, AFC is thought to reflect the number of small follicles ready to grow — not necessarily something that can be changed quickly or easily. Lifestyle factors like smoking cessation, stress management, and maintaining a healthy weight may support your overall fertility, but there’s no magic fix. If you’re concerned about a low count or want to explore your options, speak to a fertility specialist who can guide you based on the bigger picture — not just the numbers.
What does a ‘high’ antral follicle count mean?
A high antral follicle count (AFC) means your ovaries show a larger number of resting follicles than average — often more than 20 across both ovaries. This can be a positive sign, especially if you’re trying to conceive or planning IVF. A higher AFC generally means a bigger pool of eggs to work with, and in IVF, it can increase the number of eggs retrieved during stimulation.
That said, too high a count can come with caveats. It may point to conditions like polycystic ovary syndrome (PCOS) or signal hormone imbalances that affect regular ovulation. In IVF, a very high AFC may also increase the risk of ovarian hyperstimulation syndrome (OHSS), which is why treatment plans are adjusted carefully to reduce that risk. In short, a high AFC can offer more options — but it’s important to understand the context and have a team that can interpret the full picture. [17,31,32,33]
Can you have low AMH but high AFC?
Yes — and it happens more often than you might think. Around 1 in 5 people show a mismatch between their AMH levels and antral follicle count (AFC), and one of the most common patterns is having a low AMH but a high AFC.
This can feel confusing, especially if you’ve been told AMH is the go-to marker for ovarian reserve. But in cases of discordance, research suggests that AFC may give a more accurate picture of how your ovaries will respond to stimulation — particularly in the context of IVF. People with a high AFC and low AMH (sometimes due to individual variation, measurement issues, or even rare AMH gene mutations) tend to have better egg yield, embryo quality, and clinical pregnancy rates than those with the opposite pattern. [31,34]
In practical terms, a high AFC usually means there’s still a good number of recruitable follicles — even if AMH is on the lower side. If you’re preparing for fertility treatment, your clinic will likely use both markers alongside age, hormone levels, and other tests to personalise your protocol. But if there’s a clear discrepancy, it’s often the AFC that carries more weight when predicting how well your body may respond.
What happens after an antral follicle ultrasound?
After the scan, your clinician will explain your results and what they might indicate. It’s important to know that while an AFC can show how many resting follicles you have at that moment, it doesn’t predict whether or when you’ll conceive. Instead, it gives a clearer sense of how many eggs you might have left — and can flag up conditions like PCOS or signs of low ovarian reserve that may affect your reproductive plans.
Ultimately, this kind of insight adds to the bigger picture. It doesn’t offer all the answers, but it’s a valuable piece of information that can help guide your next steps — whether you’re considering treatment, looking to preserve your fertility, or simply want to understand more about your reproductive health.
Antral follicle count FAQs
How accurate is an antral follicle count?
It’s reasonably accurate — AFC is a valuable marker of ovarian reserve, especially for understanding how your body might respond to IVF. It’s particularly good at predicting the risk of cycle cancellation when counts are low (typically under four). But its ability to predict pregnancy is more limited. [35]
The scan itself is done by a trained sonographer, who counts the small follicles by eye during a transvaginal ultrasound. While they’re skilled at spotting what matters, there’s always a margin for error — especially if the follicles are very small or the scan isn’t perfectly clear. That’s why AFC works best as part of a bigger picture, alongside age, AMH, and other clinical details.
Is AMH or AFC more accurate?
AFC is generally the more accurate predictor of how your ovaries will respond to fertility treatment — especially when planning IVF. It gives a direct count of recruitable follicles, which can closely reflect how many eggs might be retrieved.
AMH still plays an important role, offering insight into longer-term ovarian reserve and being less affected by cycle timing. The two usually align, but when they don’t, AFC tends to be more reliable for treatment planning. Most clinics use both to build the clearest picture. [36]
Does AFC change month to month?
Yes, your antral follicle count (AFC) can vary slightly from cycle to cycle — and even within the same cycle. It’s most often measured during the early follicular phase (typically days 2–5) for consistency, but studies show that even when measured later in the cycle, AFC remains clinically useful. [37]
Small changes from month to month are normal and often reflect natural hormonal fluctuations or differences in scan timing. In most cases, these shifts don’t significantly impact how your fertility specialist designs a treatment plan. While AFC isn’t perfectly stable, it’s still a trusted marker — especially when interpreted alongside age, AMH, and other indicators of ovarian reserve. — since multiple pregnancies can come with a higher risk factor. [38]
How big are follicles?
Follicles grow and change size throughout your cycle, but they start small. The ones counted in an antral follicle count (if your AFC is done early in your follicular phase) are usually between 2–10mm across — roughly the size of a sesame seed to a cherry. [39]
When you’re going through fertility treatment like IVF, follicle size becomes a key focus. Most clinics aim to trigger ovulation when the lead follicle reaches about 18–22mm, as that’s when an egg is typically mature and ready for retrieval. Some studies suggest the sweet spot for higher pregnancy rates — especially with ovulation induction medications like clomiphene or letrozole — is slightly larger, around 23–28mm. [40,41,42]
That said, bigger isn’t always better. Follicles smaller than 13mm are less likely to contain mature eggs, while those over 28mm might be overripe. So, while size matters, balance is everything — and your clinic will track it closely to time things just right.
What size follicles for twins?
Follicles measuring 12mm or more may increase the chance of twins — especially if there’s more than one. Most twin pregnancies during IUI happen when there’s at least one other follicle that’s 14mm or larger. That’s why clinics may adjust or cancel a cycle if multiple follicles reach this size — since multiple pregnancies can come with a higher risk factor. [38]
Sources
- https://mft.nhs.uk/saint-marys/services/gynaecology/reproductive-medicine/what-else-do-i-need-to-know/
- https://www.sciencedirect.com/topics/medicine-and-dentistry/antral-follicle
- https://www.nice.org.uk/guidance/cg156/chapter/recommendations
- https://www.ncbi.nlm.nih.gov/books/NBK576440/
- https://www.fertstert.org/article/S0015-0282(99)00396-9/fulltext
- https://www.britishfertilitysociety.org.uk/wp-content/uploads/2015/11/Ovarian.Reserve.pdf
- https://mft.nhs.uk/saint-marys/services/gynaecology/reproductive-medicine/what-else-do-i-need-to-know/
- https://www.worcsacute.nhs.uk/documents/documents/patient-information-leaflets-a-z/you-and-your-fertility-journey/
- https://www.sciencedirect.com/topics/nursing-and-health-professions/antral-follicle-count
- https://www.sciencedirect.com/science/article/pii/S0015028224001730
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5624332/
- https://pubmed.ncbi.nlm.nih.gov/33164068/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9298690/
- https://pubmed.ncbi.nlm.nih.gov/33168492/
- https://pubmed.ncbi.nlm.nih.gov/25504940/
- https://pubmed.ncbi.nlm.nih.gov/32211797/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8421664/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3675173/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10002966/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3663963/
- https://www.sciencedirect.com/science/article/pii/S0965229920318008
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5568942/
- https://pubmed.ncbi.nlm.nih.gov/36107111/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3800538/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4229792/
- https://www.sciencedirect.com/science/article/abs/pii/S0301211512005817
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8158119/
- https://hannahpearn.com/2023/09/21/can-acupuncture-increase-ivf-success-rates/
- https://hannahpearn.com/2023/05/12/does-stress-affect-fertility/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC2821936/
- https://link.springer.com/article/10.1186/s12958-019-0497-4
- https://pubmed.ncbi.nlm.nih.gov/25302750/
- https://www.leedsth.nhs.uk/patients/resources/ovarian-hyperstimulation-syndrome-ohss/
- https://www.sciencedirect.com/science/article/pii/S2666334124000060
- https://www.ncbi.nlm.nih.gov/books/NBK76802/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3604835/
- https://www.rbmojournal.com/article/S1472-6483(16)30288-7/fulltext
- https://pubmed.ncbi.nlm.nih.gov/30482725/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6505459/
- https://www.sciencedirect.com/science/article/pii/S0015028222001364
- https://pubmed.ncbi.nlm.nih.gov/22459633/
- https://obgyn.onlinelibrary.wiley.com/doi/full/10.1002/uog.18955


