Seen / Resources / Fertility Conditions / Arcuate Uterus: What It Means for Fertility, Pregnancy, and Trying to Conceive
Arcuate Uterus: What It Means for Fertility, Pregnancy, and Trying to Conceive
An arcuate uterus is one of the most common uterine shape variations — but many don’t know how it can impact them. If you’ve recently been diagnosed, this guide will help you understand what it means for fertility, pregnancy, and next steps.

Author
Tassia O’Callaghan

Reviewed by
Kayleigh Hartigan
23 min read
Spotlight:
- An arcuate uterus is a mild, congenital variation in uterine shape and is often considered a normal anatomical variant.
- It’s present from birth, doesn’t change over time, and usually doesn’t need treatment.
- Most people with an arcuate uterus have normal fertility and pregnancy outcomes, especially when no other factors are present.
- Current research shows no reduction in pregnancy rates, including with IVF or IUI, though evidence on later pregnancy outcomes is mixed, and more research is needed.
- Diagnosis is best confirmed with 3D ultrasound, as arcuate uterus can sit in a diagnostic grey zone.
What is an arcuate uterus?
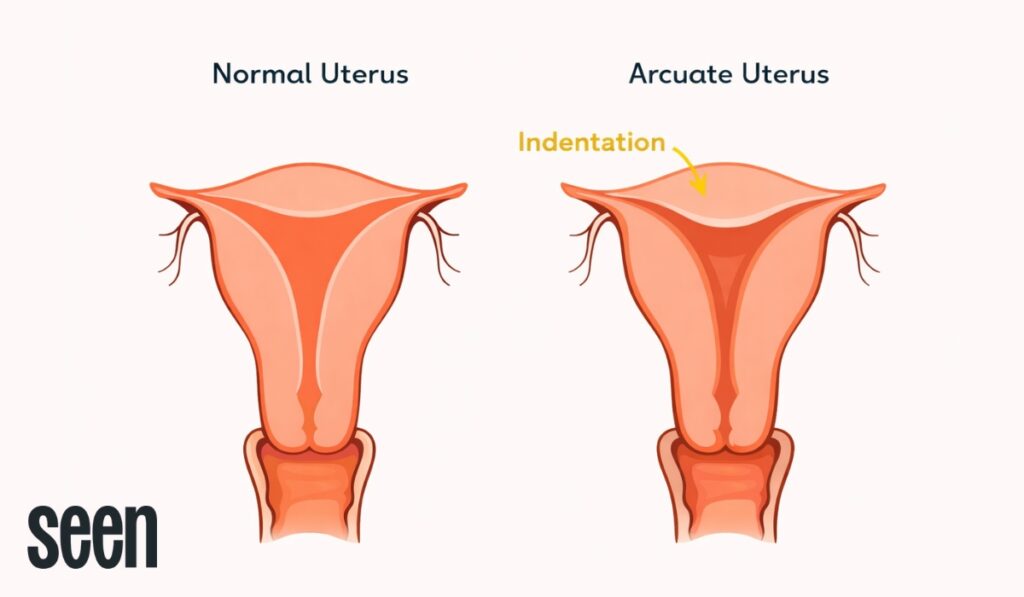
An arcuate uterus is a mild, congenital variation in the shape of the uterus. Rather than having a completely flat or gently curved top (known as the fundus), the uterus has a small inward dip at the top. This dip is shallow and smooth, which is an important distinction — it’s what separates an arcuate uterus from other uterine anomalies like a septate or bicornuate uterus, where the shape difference is more pronounced and clinically significant.
An arcuate uterus is present from birth and doesn’t change, progress, or worsen over time. Because of this, it’s often described as a “normal” anatomical variant, rather than a structural abnormality that needs fixing. In fertility medicine, it sits at the mildest end of the uterine anomaly spectrum, and for many people, it has little to no impact on fertility or pregnancy outcomes.
What does it mean if you have an arcuate uterus?
For most people, having an arcuate uterus doesn’t meaningfully change how conception or pregnancy is approached. It’s considered a mild variation in uterine shape, and in many cases it doesn’t interfere with ovulation, implantation, or the ability to carry a pregnancy. Because of this, it’s often managed with reassurance rather than intervention.
Many people only discover they have an arcuate uterus incidentally. It’s commonly picked up during fertility investigations, following investigations for recurrent pregnancy loss, or during more detailed imaging such as a 3D ultrasound or MRI. In other words, it’s often found because clinicians are looking closely — not because it was causing symptoms or problems on its own.
If you’ve been told your uterus is “mildly arcuate,” that wording really matters. Mild arcuate uteri are widely considered compatible with normal fertility and pregnancy outcomes, and most professional guidelines do not classify them as a high-risk finding. For many people, the diagnosis becomes a piece of background information rather than something that dictates next steps — helpful to know, but not something that defines or limits your fertility path. [1]
How rare is an arcuate uterus?
An arcuate uterus is not considered rare. Congenital uterine anomalies (CUAs) as a group are estimated to affect between 5 to 10% of women and birthing people, according to data shared by Tommy’s. An arcuate uterus is one of the most common and mildest variations within this group, potentially affecting around 3 to 3.9% of the female population. [2,3,4]
CUAs are identified more often in people who have experienced pregnancy loss or fertility challenges. Rates are estimated to be around 17 in 100 among those with recurrent miscarriage, and up to 25 in 100 in people with a history of both miscarriage and infertility. This doesn’t mean the uterine shape is always the cause, but rather that more detailed imaging is often performed in these situations, increasing the likelihood of a diagnosis. [2]
In the wider population, many people with an arcuate uterus never know they have one. It often goes undetected because it doesn’t usually cause symptoms or problems, and is typically only picked up when scans are done for another reason.
When to See a Fertility Doctor: Signs, Timelines, and What to Expect
Knowing when to see a fertility doctor can help you take control of your family-building plans with confidence.
What causes an arcuate uterus?
An arcuate uterus develops during foetal development, at the stage when your uterus is forming from two structures called the Müllerian ducts. In typical development, these ducts fuse together and then remodel to create a smooth, unified uterine cavity. With an arcuate uterus, that process of fusion happens as expected, but the final remodelling step is almost complete rather than perfectly flat. The result is a small, smooth indentation at the top of the uterus. [5,6]
Because this happens before birth, an arcuate uterus is classed as a congenital uterine anomaly (CUA). That wording can sound more alarming than it needs to be. In clinical practice, an arcuate uterus is usually understood as a normal anatomical variation rather than a structural problem, sitting at the mildest end of the uterine anomaly spectrum. It doesn’t progress, worsen, or change over time — it’s simply the way the uterus formed.
What does not cause an arcuate uterus
It’s equally important to be clear about what doesn’t cause an arcuate uterus. There’s no evidence linking it to hormonal imbalance, lifestyle factors, infections, or anything you did or didn’t do. It isn’t caused by endometriosis, adenomyosis, or pregnancy loss, and it can’t develop later in life as a result of fertility treatment or miscarriage.
You didn’t cause this, and you couldn’t have prevented it.
You may come across reports of an arcuate uterus is found alongside other gynaecological conditions. While these overlaps can raise understandable questions, current evidence does not support a causal relationship. In most cases, the conditions are considered to be coexisting rather than connected, identified simply because more detailed imaging was performed. [7]
Can endometriosis cause arcuate uterus?
No, endometriosis doesn’t cause an arcuate uterus. These are two entirely separate conditions that arise in different ways and at different points in life.
An arcuate uterus is a congenital variation, meaning it forms during foetal development and is present from birth. Endometriosis, by contrast, is an inflammatory condition that develops later, where tissue similar to the lining of the uterus grows outside the uterine cavity. Because of this, endometriosis cannot alter the shape of the uterus in a way that creates an arcuate contour. [6]
The two conditions can, however, coexist. This is usually because people being investigated for pain, infertility, or pregnancy loss often undergo more detailed imaging, increasing the likelihood that an arcuate uterus is identified incidentally. When both are present, clinical focus is typically placed on managing endometriosis, as it is far more likely to affect symptoms, fertility, or pregnancy outcomes than the arcuate uterus itself.
What are the symptoms of an arcuate uterus?
Most people with an arcuate uterus have no symptoms at all. It’s commonly identified incidentally during scans performed for another reason, such as fertility investigations or pregnancy care, rather than because it causes day-to-day physical symptoms. This is consistent with wider guidance on congenital uterine anomalies, which notes that many people remain entirely asymptomatic. [2,8]
When symptoms or complications are reported, they are not always directly caused by the arcuate uterus itself. The challenge is that research into minor congenital uterine anomalies is limited, and much of the available evidence shows associations rather than clear cause-and-effect relationships. As a result, findings need to be interpreted carefully and always in the context of the individual.
Possible — but uncommon and inconsistently reported — associations include:
- Recurrent pregnancy loss, particularly later losses, although current evidence does not show that an arcuate uterus alone is a definitive cause. In many cases, other contributing factors are present. [3]
- Late miscarriage, preterm birth, or preterm premature rupture of membranes (PPROM). Some retrospective studies have reported higher rates of these outcomes, while others have not found significant differences. There is currently no consensus on whether an arcuate uterus independently increases risk. [1,2]
- Fetal growth restriction (FGR) and abnormal placental cord insertion, which have been observed in some studies, but again without clear evidence that the uterine shape itself is the cause rather than a contributing or coincidental finding.
- Breech or non-head-down presentation, thought to relate to subtle differences in uterine contour later in pregnancy, rather than issues with implantation or early development. [2]
- Menorrhagia (heavy periods) or amenorrhoea, although these symptoms are not typical of an arcuate uterus and should prompt assessment for other gynaecological causes. [3]
- Subfertility, which may be present in some people with congenital uterine anomalies overall, but is not clearly attributable to arcuate uterus alone. [3]
- Blood clotting issues, which have been mentioned in some pregnancy-focused resources, but without strong evidence that an arcuate uterus directly causes clotting disorders. [2]
It’s important to underline that research in this area is still evolving. While some studies suggest associations between arcuate uterus and certain pregnancy complications, researchers have not been able to confirm whether the uterine shape itself causes these outcomes. Larger, higher-quality studies are needed to draw firm conclusions.
If you’re experiencing symptoms such as heavy bleeding, absent periods, pain, or repeated pregnancy complications, it’s important not to assume they’re due to an arcuate uterus alone. In these cases, further assessment is usually recommended to look for other gynaecological, hormonal, or obstetric factors that may better explain what you’re experiencing — and to ensure you’re getting care that reflects your full clinical picture.
Can an arcuate uterus affect fertility?
Current evidence suggests that an arcuate uterus does not significantly reduce fertility. It’s generally viewed as a mild variation in uterine shape rather than a condition that interferes with reproductive function.
From a biological perspective, this makes sense. Ovulation is unaffected, as the ovaries and hormonal signalling involved in releasing an egg are independent of uterine shape. Implantation is also usually unaffected, because the shallow indentation seen in an arcuate uterus does not significantly disrupt the endometrial lining or reduce the available space for an embryo to implant. As a result, time to pregnancy for people with an arcuate uterus is generally comparable to that of the wider population, assuming no other fertility factors are present.
Arcuate uterus and miscarriage
This is where the evidence becomes more nuanced — and understandably more emotionally charged. Research into minor congenital uterine anomalies, including arcuate uterus, is still limited, and findings across studies are not always consistent. Some studies have suggested possible associations with later pregnancy complications, while others have found no meaningful differences in miscarriage risk when compared with people who have a typical uterine shape. [9]
What we do know is reassuring in key areas. In studies looking at people undergoing assisted reproductive treatment, first-trimester miscarriage rates in those with an arcuate uterus were similar to those seen in people with a normal uterine cavity. In contrast, significantly higher miscarriage rates were observed in people with major uterine anomalies, such as septate or unicornuate uterus — highlighting an important distinction between mild and more severe uterine differences. This suggests that an arcuate uterus behaves very differently from uterine anomalies that are known to affect early pregnancy outcomes. [9]
Context matters greatly. Outcomes can vary depending on whether the uterine shape has been accurately classified as arcuate rather than a small septum, which carries a very different risk profile. Other factors — including age, adenomyosis, fibroids, cervical length, placental factors, or a history of late pregnancy loss — are often far more influential in determining miscarriage or preterm birth risk than the arcuate uterus itself.
Taken on its own, an arcuate uterus is not considered a high-risk finding for miscarriage, particularly in early pregnancy. When concerns do arise, they’re best explored as part of a broader, individualised assessment rather than being attributed to uterine shape in isolation. Clear diagnosis, careful interpretation of the evidence, and personalised care are key to keeping risk in proportion — and support where it’s genuinely needed.
How to Choose the Best Fertility Clinic
Ready to find the right fertility clinic for you? Explore costs, treatments, success rates, and real patient experiences — all in one place.
What tests diagnose arcuate uterus?
An arcuate uterus is diagnosed using imaging tests that allow clinicians to assess both the shape of the uterine cavity and the contour of the fundus. This matters because the difference between a typical uterus and an arcuate uterus can be very subtle — and current classification systems acknowledge that this distinction is not always clear-cut. In fact, even with modern criteria, arcuate uterus often sits in a recognised diagnostic grey zone, which is why imaging quality and specialist interpretation are so important. [9]
- Pelvic ultrasound is often the first place an arcuate uterus is suspected. This is usually a transvaginal scan and may show a shallow indentation at the top of the uterine cavity. While useful as an initial assessment, standard two-dimensional ultrasound can miss subtle contour differences and may not be sufficient to confidently classify minor uterine anomalies.
- 3D ultrasound is considered the gold standard for diagnosing and subclassifying uterine anomalies. Using three-dimensional transvaginal imaging, clinicians can assess uterine morphology in line with recognised criteria. Because normal uterine morphology and arcuate uterus can overlap, some centres also use additional definitions to help distinguish between a straight or convex cavity (typical uterus) and a shallow concave cavity that does not meet criteria for a septate uterus. This level of detail is not possible with standard imaging.
- MRI may be used when ultrasound findings are unclear or when there is disagreement between reports. MRI provides high-resolution images of both internal and external uterine anatomy and can be helpful in complex cases, particularly when it’s important to rule out a septate, bicornuate, or other major Müllerian anomaly.
- Hysteroscopy is sometimes performed during fertility or miscarriage investigations, but it has important limitations in this context. While it allows direct visualisation of the uterine cavity, it does not show the external fundal contour. This means subtle anomalies — such as an arcuate uterus — can be missed or misclassified when hysteroscopy is used alone.
A 3D ultrasound is particularly valuable because it helps distinguish an arcuate uterus from a septate uterus, which is a critical distinction. A septate uterus is defined by a deeper endometrial septum (typically greater than 1 cm with a narrow angle) and carries a very different risk profile, including higher miscarriage rates and potential benefit from surgical treatment. An arcuate uterus, by contrast, usually does not require intervention. [1,3,9]
Because uterine anomalies can be complex — and because minor anomalies like arcuate uterus are increasingly identified with better imaging — referral to gynaecology or fertility specialists for 3D ultrasound is recommended when a uterine abnormality is suspected. Diagnosis may be made by a gynaecologist, fertility specialist, or radiologist with expertise in pelvic imaging, and in many fertility settings, scans are reviewed by more than one clinician to ensure the classification is accurate before any management decisions are made.
This careful, proportionate approach helps avoid both overdiagnosis and overtreatment — while ensuring that clinically meaningful anomalies are not missed.
Can you treat an arcuate uterus?
In most cases, no treatment is required for an arcuate uterus. Because it’s considered a mild anatomical variation rather than a structural abnormality, management usually focuses on reassurance and accurate diagnosis rather than intervention.
Surgical correction, most commonly referred to as hysteroscopic metroplasty, is generally not recommended for an isolated arcuate uterus. Current evidence shows that surgery does not improve fertility or pregnancy outcomes in people with an arcuate uterus alone, and when the uterine anatomy is otherwise normal, surgery introduces unnecessary risk. These risks can include infection, bleeding, uterine scarring, or complications in future pregnancies, without a clear benefit to justify them. [10]
That said, treatment may occasionally be discussed in very specific circumstances. This is most often when there is diagnostic uncertainty between an arcuate uterus and a septate uterus, as a septum carries a different risk profile and may benefit from surgical treatment. In some cases, a history of unexplained late pregnancy loss may prompt further discussion, particularly if imaging suggests the indentation is deeper than expected. Rarely, a specialist may feel that the indentation is functionally significant, meaning it could plausibly affect pregnancy outcomes, although this is uncommon. [11]
Even in these situations, decisions are made carefully and on an individual basis. Specialists tend to take a conservative approach, weighing the potential risks and benefits in the context of your full medical and reproductive history, rather than recommending treatment based on uterine shape alone.
How to conceive with an arcuate uterus
If you’re trying to conceive with an arcuate uterus, the starting point is understanding that this diagnosis rarely dictates how conception should happen. Current evidence suggests that an arcuate uterus doesn’t reduce the chances of conceiving, including when fertility treatment is used. Where the research is less clear is around pregnancy outcomes later on — which means planning should be thoughtful, but not overly cautious. [6]
- Ensure the diagnosis is accurate, ideally using three-dimensional transvaginal ultrasound. Because arcuate uterus sits close to the boundary between typical and atypical uterine shapes, precise imaging helps avoid misclassification and ensures that conditions with different management — such as septate uterus — are not missed.
- Assess fertility more broadly, including ovulation, sperm health, and fallopian tube function. When conception is delayed, these factors are much more likely to explain why than the presence of an arcuate uterus itself.
- Proceed with unassisted conception where appropriate, as most people with an arcuate uterus conceive without intervention. There is no evidence to support delaying attempts to conceive or pursuing treatment solely because of this finding.
- Use cycle awareness tools if they add clarity, whether through at-home tracking or clinic-based monitoring. For some people, this provides reassurance and helps optimise timing, particularly when navigating uncertainty around fertility.
- Seek specialist input if pregnancy hasn’t occurred within expected timeframes, based on age and individual circumstances. Referral criteria are the same as for people without uterine anomalies, and an arcuate uterus alone does not usually accelerate the need for treatment.
It’s also worth separating conception from pregnancy outcomes. While some studies have explored whether an arcuate uterus may be linked to later pregnancy complications, results are mixed and sample sizes are small. Importantly, infertility treatment success rates appear comparable to those seen in people with a typical uterine shape. For most, the priority is not correcting uterine anatomy, but ensuring good-quality diagnosis, appropriate follow-up, and care that reflects the whole clinical picture — not a single scan finding. [1]
How does arcuate uterus affect fertility treatment?
If you’re considering or already undergoing fertility treatment, it’s natural to wonder whether an arcuate uterus will change how treatment is planned or how successful it might be. The reassuring answer, in most cases, is that it doesn’t. Because an arcuate uterus is considered a mild anatomical variation, fertility clinics generally treat it as background information rather than a factor that dictates protocol. Decisions around treatment type, medication, and timing are usually guided by the same considerations used for anyone else, like age, ovarian reserve, sperm parameters, and overall reproductive history. [1,6]
IVF and IUI with an arcuate uterus
When it comes to IVF and IUI, the evidence is reassuring around treatment success. Studies consistently show that having an arcuate uterus does not reduce conception or implantation rates with assisted reproductive technologies, and pregnancy rates following treatment appear comparable to those seen in people with a typical uterine shape. Because the external contour of the uterus is normal and the cavity change is shallow, procedures such as embryo transfer are rarely technically difficult, and clinics generally proceed without modifying stimulation plans or transfer technique. [1]
Where the research is less settled is what happens later in pregnancy, rather than whether treatment works in the first place. Some observational studies have explored whether minor uterine shape variations are linked to certain perinatal outcomes, but these findings don’t translate into changes in how IVF or IUI is delivered. Importantly, there is no evidence to support additional medication, altered protocols, or preventative intervention at the treatment stage based on an arcuate uterus alone. [1]
In practice, fertility teams focus on the factors that most strongly influence treatment outcomes — egg quality, sperm parameters, embryo development, and timing — while keeping uterine morphology in context. For most people, an arcuate uterus is noted, not acted upon, during IVF or IUI planning, with attention shifting to pregnancy monitoring only if individual risk factors or previous outcomes suggest it’s appropriate.
Egg freezing with an arcuate uterus
An arcuate uterus has no impact on egg freezing. Egg freezing outcomes and ovarian stimulation protocols are determined by ovarian function and hormonal response, not uterine shape. If egg freezing is part of your fertility plan, the presence of an arcuate uterus doesn’t change how this treatment is approached or its expected outcome. [12]
Pregnancy monitoring with an arcuate uterus
After pregnancy is established — whether spontaneously or with fertility treatment — care is usually shaped by individual risk factors rather than diagnosis alone. While many people with an arcuate uterus go on to have uncomplicated pregnancies, some studies have reported higher rates of outcomes such as spontaneous preterm birth, fetal growth restriction, and cervical shortening. At the same time, the research is mixed, sample sizes are often small, and findings aren’t consistent enough to justify a one-size-fits-all approach. [2,8,13,14,15]
In practice, this means monitoring is often proportionate and responsive. Some care teams may offer additional reassurance scans in early pregnancy, assess cervical length during the second trimester, or recommend consultant-led antenatal care — particularly if there’s a history of late miscarriage, preterm birth, or other relevant risk factors. In the UK, known uterine variants (including arcuate uterus) are commonly considered when deciding whether referral to a preterm birth or specialist antenatal clinic is appropriate, not because complications are expected, but because early planning can be helpful. [15]
Importantly, closer follow-up doesn’t mean something is “wrong.” It reflects an awareness that uterine shape is one piece of a much larger picture. For many people, pregnancy care proceeds in the same way it would without this diagnosis, with adjustments made only if and when there’s a clear clinical reason to do so.
Find the right clinic for you
Choosing a clinic is one of the biggest decisions you’ll make. We’ll find the best options for you and arrange your pre-treatment tests, empowering you from this point onwards.
Is an arcuate uterus high risk?
For most people, the answer is no. An arcuate uterus is not automatically classed as a high-risk fertility or pregnancy condition, and on its own it does not usually change standard care or management. In many cases, it’s treated as background information rather than something that defines how a pregnancy will unfold.
That said, pregnancy care is always individualised. Your care team may take your uterine shape into account alongside other factors, particularly if you have a history of later pregnancy loss or preterm birth. In these situations, they may choose to monitor cervical length later in pregnancy, offer additional growth scans, or review your obstetric history more closely to ensure any emerging risks are picked up early. These steps are precautionary and focused on reassurance rather than expectation of problems. [2,8,13,14,15]
Crucially, risk assessment is based on your whole clinical picture, not the uterine shape alone. Factors such as age, previous pregnancy outcomes, co-existing gynaecological conditions, and overall health tend to play a far larger role in determining risk than an arcuate uterus by itself.
Arcuate uterus: What this diagnosis really means for your fertility path
An arcuate uterus can sound more serious than it usually is. While the diagnosis often raises understandable questions, it’s widely considered one of the mildest uterine shape variations and is generally compatible with normal fertility and healthy pregnancy outcomes. For most people, it doesn’t require treatment, doesn’t automatically increase risk, and doesn’t change the fundamentals of how conception or fertility treatment is approached.
What can make a meaningful difference is having the right clinical support around you. A fertility clinic that takes the time to interpret your scans accurately, place the finding in context, and look at your fertility as a whole can help remove unnecessary worry and avoid overtreatment. That’s where choosing the right clinic matters — not just for access to treatment, but for clear explanations, proportionate care, and confidence in the decisions you’re making.
If you’re exploring your options, our free Clinic Match tool can help you find clinics with the right expertise for your individual situation. Because with an arcuate uterus, clarity and personalised care — not correction — are usually what move things forward.
Arcuate uterus FAQs
What is the pregnancy rate for arcuate uterus?
Overall, the available evidence suggests that having an arcuate uterus does not lower your chances of becoming pregnant, including if you’re trying through assisted reproductive treatment. Large studies in people undergoing ART have found pregnancy rates in those with an arcuate uterus to be comparable to — and in some cases slightly higher than — those seen in people with a typical uterine shape. This supports the understanding that an arcuate uterus does not usually disrupt ovulation, fertilisation, or early implantation. [4,9]
Where the picture becomes less clear is later in pregnancy, not at the point of conception. Research in this area is limited, and while some studies have explored links with later pregnancy outcomes, they don’t show a consistent reduction in the ability to conceive. In practice, if pregnancy isn’t happening as expected, clinicians are far more likely to look at other fertility factors first, rather than attributing delays to the uterine shape alone. [9]
Is arcuate uterus the same as septate uterus?
No — and this distinction is really important. A septate uterus has a fibrous or muscular partition that divides the uterine cavity, which is associated with a higher risk of miscarriage and may benefit from surgical treatment. An arcuate uterus, by contrast, has only a shallow indentation at the top of the cavity and does not divide it. Because management and risk profiles differ significantly, accurate diagnosis — often with 3D ultrasound — is key.
Can you have a successful pregnancy with an arcuate uterus?
Yes. Many people with an arcuate uterus go on to have healthy, full-term pregnancies without complications related to uterine shape. For most, the diagnosis doesn’t change how pregnancy progresses or how it’s managed. When additional monitoring is offered, it’s usually precautionary and based on individual history rather than expectation of problems. The presence of an arcuate uterus alone does not prevent a positive pregnancy outcome.
Which uterus is not good for pregnancy?
Certain uterine shapes can be more strongly associated with adverse pregnancy outcomes, including septate uterus, bicornuate uterus, and unicornuate uterus. These variants can affect implantation, growth, or space within the uterus and may require specialist input. An arcuate uterus is not usually included in this group, as it’s considered the mildest variation and is widely compatible with successful pregnancy.
Sources
- Yoshihara, T., Okuda, Y. and Yoshino, O., 2025. Diagnosis of arcuate uterus using three‐dimensional transvaginal ultrasound and investigation of its association with perinatal complications. International Journal of Gynecology & Obstetrics, 168(3), pp.1073-1078.
- Tommy’s. Congenital uterine abnormalities (differently-shaped womb). Reviewed 15 January 2025.
- NHS North East London. Community Gynaecology Guidelines. January 2025.
- Chan YY, Jayaprakasan K, Zamora J, Thornton JG, Raine-Fenning N, Coomarasamy A. The prevalence of congenital uterine anomalies in unselected and high-risk populations: a systematic review. Hum Reprod Update. 2011 Nov-Dec;17(6):761-71. doi: 10.1093/humupd/dmr028. Epub 2011 Jun 24. PMID: 21705770; PMCID: PMC3191936.
- Wilson D, Bordoni B. Embryology, Mullerian Ducts (Paramesonephric Ducts). [Updated 2023 Mar 6]. In: StatPearls [Internet].
- Royal College of Obstetricians & Gynaecologists. Reproductive Implications and Management of Congenital Uterine Anomalies (2024 Second Edition) (Scientific Impact Paper No. 62). Last reviewed 21 November 2019.
- Rana, L., Sood, D., Rana, N. and Singh, D., 2020. Arcuate Uterus with Focal Cystic Adenomyosis-A Case Report. OSP Journal of Case Reports, 2(4), pp.1-2.
- NHS Scotland. Congenital uterine anomalies (951).
- Jayaprakasan, K., Chan, Y.Y., Sur, S., Deb, S., Clewes, J.S. and Raine‐Fenning, N.J., 2011. Prevalence of uterine anomalies and their impact on early pregnancy in women conceiving after assisted reproduction treatment. Ultrasound in obstetrics & gynecology, 37(6), pp.727-732.
- Ludwin, A. and Pfeifer, S.M., 2019. Reproductive surgery for müllerian anomalies: a review of progress in the last decade. Fertility and Sterility, 112(3), pp.408-416.
- Carbonnel M, Pirtea P, de Ziegler D, Ayoubi JM. Uterine factors in recurrent pregnancy losses. Fertil Steril. 2021 Mar;115(3):538-545. doi: 10.1016/j.fertnstert.2020.12.003. PMID: 33712099.
- Roque M, Sunkara SK. The most appropriate indicators of successful ovarian stimulation. Reprod Biol Endocrinol. 2025 Jan 9;23(Suppl 1):5. doi: 10.1186/s12958-024-01331-6. PMID: 39789602; PMCID: PMC11714799.
- Connolly CT, Hill MB, Klahr RA, Zafman KB, Rebarber A, Fox NS. Arcuate Uterus as an Independent Risk Factor for Adverse Pregnancy Outcomes. Am J Perinatol. 2024 Jan;41(2):167-173. doi: 10.1055/a-1674-5927. Epub 2021 Oct 20. PMID: 34670319.
- Kugelman N, Gangbe EM, Badeghiesh A, Baghlaf H, Dahan MH. Pregnancy and neonatal outcomes in women with arcuate uterus: a population-based cohort study of over 3.8 million women. BMC Pregnancy Childbirth. 2025 Oct 28;25(1):1143. doi: 10.1186/s12884-025-08125-7. PMID: 41152778; PMCID: PMC12560325.
- NHS University Hospital Southampton, NHS Foundation Trust. Referral to the preterm birth clinic.